Choosing to die

Right-to-die legislation will go into effect this year in California, which will join Oregon, Montana, Vermont, and Washington in providing for physician-assisted suicide. According to a Gallup poll last year, 70 percent of Americans believe that doctors should be allowed to help terminally ill patients end their lives—and that figure has been on the rise for several years.
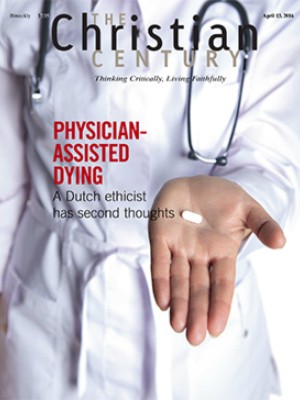
In this issue, two writers take a hard look at the practice of physician-assisted dying. Both tell cautionary tales.
Dutch ethicist Theo Boer examines the effect of laws in the Netherlands in place since 1994 which have allowed physicians to assist in deaths. He argues that once laws permitting physician-assisted dying are established, they change people’s expectations in facing death. Once the door to assisted death is opened, it seems, it’s difficult to keep it from opening further.
Read our latest issue or browse back issues.
Boer, who reviewed many cases of physician-assisted death in the Netherlands as part of a government panel, noticed that the number of physician-assisted deaths began rising sharply in 2007. Requests were coming not only from terminally ill patients in extreme pain—the expected profile—but from people who might otherwise live for years.
Joseph Kotva probes the results of the 1994 right-to-die law in Oregon, which pioneered physician-assisted dying in the United States. Like Boer, Kotva notes that a strong concern for autonomy and self-sufficiency undergirds support for physician-assisted death. He finds that those seeking to end their lives were less likely to have intimate and trusting relationships, and they often perceived themselves as having few social supports.
The Netherlands presents an irony when it comes to the notion of individual autonomy: given a choice between having a physician administer a lethal dose (euthanasia) or having the physician merely provide a lethal dose (physician-assisted suicide), 95 percent choose euthanasia. They prefer that death come literally at the hands of another.
These articles should lead Christian communities to reflect on their own practices of care for the dying. The church has long been a central place for practices that address the isolation and the fear of isolation that often come at the end of life. It can be both a space for difficult conversations about choices at the end of life and a place for communal care.
No matter how compassionate a community of care is, two critical questions remain: Where assisted dying becomes legal, can it be limited in such a way as not to undermine human solidarity and the holiness of every life? Where assisted dying is prohibited, can communal practices of medical and pastoral care be robust enough to prevent people from dying in loneliness, pain, and despair?