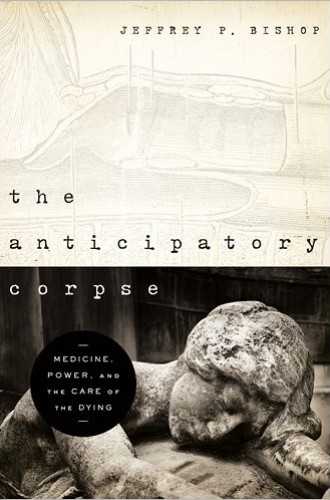
Can medicine be cured?
In this brilliant book, Jeffrey Bishop, who is both a physician and a philosopher, turns his clinical and analytical gaze on medicine. His diagnosis is bleak: “There is something rotten in the heart of medicine.” Nine of the ten chapters are devoted to the diagnosis, showing the source and history of the disease and some of its symptoms, always focusing on how medicine approaches death and care for the dying. These chapters demand patience from the reader, but they are important not only for physicians but also for those of us who are or will be their patients. In the last chapter, he turns his attention to therapeutic possibilities for medicine and raises a series of provocative questions, the most provocative of which is the last line of his book: Might it not be that only theology can save medicine?
Bishop begins with etiology, with a history of the causes and origins of the disease that has infected medicine. He briefly acknowledges the influence of Francis Bacon’s account of knowledge as power over nature and over its threats of death and suffering. Then, following Michel Foucault’s account of the genealogy of modern medicine in The Birth of the Clinic, he focuses on the work of Claude Bernard, whose “clinical gaze” upon the dead body in autopsy (and vivisection) became foundational for medicine. In the 19th century, the dead body, the corpse, became “the epistemologically normative body,” the body by which other bodies are known. The clinical gaze upon the body as an object to be measured and manipulated came to characterize medical care of living and diseased bodies.
Read our latest issue or browse back issues.
Because purpose and telos can hardly be ascribed to a corpse, this new epistemology for medicine provided as a corollary “the metaphysics of efficient causation.” Together they turned the patient from “subject” to “object,” dismissed the particularity of patients and rejected any attention to purpose and a final telos in life. They allowed for, and called for, medicine’s sovereign dominion over death and dying.
Important to Bishop is Foucault’s notion of “biopolitics.” Medicine becomes the way to govern our bodies, not only for their own good but also for the good of the body politic. Medicine wins the support of government—which has charge of public health—not so much by coercively restraining our desires as by shaping and disciplining them.
Here another strand of “scientific” medicine became important, one based not on physiology but on statistics. Statistical medicine garnered the interest of governments, insurance companies, eugenicists, and not least a set of new “experts,” the psychological and social scientists. Statistical medicine allowed for, and called for, a new ethic for medicine—a utilitarian calculus of the greatest good for the greatest number.
Symptomatically, medicine’s disease was expressed in the medicalization of death. Impressed by medicine’s successes, physicians and others imagined death as the great enemy to be defeated by the greater powers of medicine. But death will not finally be defeated by medicine, and in resisting death medicine sometimes does violence. There can be violence in routine cardiac-pulmonary resuscitation efforts and in other measures to force dying life to stay alive. Violence is also done to patients and their families when dying is reduced to a matter of physiology and medical control, demeaning any sense of the meaning and purpose of life. If all that is seen in the clinical gaze is death as the terminus in a series of physiological causes and effects, then life and death have no meaning.
Protests were lodged against the medicalization of death, but the protests and proposed remedies were formed (or de-formed) by the emphasis within liberal society upon the “autonomous self” and by medicine’s claim to sovereignty over death. One successful protest insisted on the patient’s right to reject technological interventions. That move, however, only managed to transfer sovereignty to the patient; it did not alter medicine’s epistemology or supply a different imagination concerning death.
A second protest and a remedy—one proposed by Drs. Jack Kevorkian and Timothy Quill and enacted by the Netherlands and the state of Oregon—legitimate physician-assisted suicide, as if “a properly authorized decision” and medical involvement make this kind of death morally acceptable. Bishop argues convincingly that medicine’s metaphysic of efficient causation has undercut the traditional (and still warranted) distinction between killing and letting die. He warns that when death is made an option in policies designed to maximize freedom and control, we may lose the option of staying alive without having to justify our existence.
Bishop also examines the definition of death as “whole brain death” and the use of that definition in the service of organ transplantation. He is suspicious of defining death as a definitive point in time and as located in the brain; death is more mysterious than that. He is cleverly critical of the confusion in our language, as when we say that a “healthy corpse” is on “life-saving equipment” and ready for the removal of organs. He is suspicious of practices in which the “living bodies of the dead” are harvested for the sake of “the dying bodies of the living,” including those practices in which regulatory agencies and transplantation centers collaborate in the interest of the medicine’s efficiency and control over death. He is critical of the dualism that reduces bodies to machines with replaceable parts and that reduces persons to their capacities for decision.
In such cases, medicine’s malady is expressed in the violence inflicted on families when transplantation medicine with its commitment to efficient control over death organizes things in the interest of harvesting the organs. Family and friends are then given “no time to pause with the dying [or dead] before the gravity of living and dying.” No attention is then paid to the desire to show proper respect for the mortal remains of the beloved one who is dying (or dead), the one whose body remains the site of respect and care in the mysterious continuity and discontinuity of those mortal remains with the beloved person.
Bishop does not want, I think, to eliminate transplantation medicine, but it is not clear what line he would draw to mark some point for the permissible harvesting of organs. This much is clear: he wants to limit medicine’s drive to manipulate and control, and as suspicious as he is of the whole brain definition of death, he warns against locating death not in the brain but in decision. Then transplantation becomes a form of “justified killing,” justified because the person making the choice is authorized as the “proper sovereign.” Such choices may soon become not only justified but “morally required” in order to give the gift of life to another.
Bishop provides a brilliant and sad account of the debate over Terri Schiavo and other patients in a persistent vegetative state. Bishop is critical of both the “social liberals” who insisted that life and death are matters of sovereign decision and of the “social conservatives” who insisted on the political rights of “bare life,” of life reduced to mechanical physiological function. He is critical of both camps for their readiness to invoke the courts, surrendering to them decisions that properly belong to particular households and communities. Moreover, neither side seemed capable of mourning the ambiguity of what they were advocating or acknowledging the tragedy involved, whatever was decided.
In perhaps the most startling and provocative section of the book Bishop turns his attention to palliative medicine. It is, of course, a response from within medicine to the medicalization of death. It recognizes that the mastery of death through technological control has eluded medicine, and it is sometimes celebrated as a remedy not only for medicalization but also for the malady of medicine that Bishop traces to medicine’s epistemology.
In Bishop’s account, however, palliative medicine is also infected. If medicine cannot defeat death by technology, it will master the uncertainties of dying by the expert discourses of psychology and sociology. Here the statistical medicine that Foucault already observed as important to “biopolitics” deploys technologies of assessment to examine and control the human experience of dying. A shift is made from a biomedical model to a “biopsychosocialspiritual” model of medicinal control, but medicine remains an effort at technological control. “Biopsychosocialspiritual medicine measures all things and is the measure of all things.” Palliative medicine is not just holistic care; it is total and totalizing care. The “metaphysics of efficient causation” remains in effect, now focused on an efficient and prompt transition through something like Elizabeth Kubler-Ross’s “stages of dying” to “acceptance.”
Bishop acknowledges the continuity of palliative medicine with the work of Cicely Saunders, the founder of the modern hospice movement. But it is the discontinuity that he emphasizes. There is a discontinuity between her vision, animated by Christian traditions and practices of charity and hospitality, and the vision of efficient control he attributes to palliative medicine. It is the difference between an imagination formed by Matthew 25, which privileges the sick and dying, and an imagination formed by medicine’s (and biopolitics’) confidence in the gaze of the expert. Palliative medicine, according to Bishop, has mutated from its beginnings in Saunders’s vision, infected by medicine’s malady.
Finally, in the last chapter, Bishop turns to therapy for medicine’s disease. He hesitates to “prescribe” solutions, not only because, as he says, “diagnosis is easy; therapy is difficult,” but also because medicine so frequently co-opts solutions, rendering them part of medicine’s efficient control. Still, there is a proposal here, a radical proposal that calls for nothing less than reimagining medicine.
If “death’s dominion becomes medicine’s dominion,” it is no wonder he titles the concluding chapter “Anticipating Life.” And if anticipating life is key to reimagining medicine, it is little wonder that he finally wonders, “Might it not be that only theology can save medicine?”
Bishop does not suddenly adopt an explicitly theological voice, but he invites it and finally admits he needs it. He wants to reimagine medicine by setting it in the context of a larger telos in which death is not simply a terminus, in which life is acknowledged as a great good but not as the ultimate good, and in which death remains an enemy, but life has the last word. He wants to set medicine in the context of a sense of our embodiment, refusing to reduce our bodies to mere physiology or our personhood to capacities for rational choice and control. He wants to set medicine in the context of a humble recognition of the limits of medicine’s powers and the tragic character of decisions to use those powers or to reject them. He wants to set medicine in the context of a story that can nurture a compassion ready to be with others in their suffering even when medicine cannot eliminate it. He wants to reimagine medicine in the context of a story that can nurture hospitality to the dying.
One could wish that he would have said more about each of these items or that he would have spoken with a more explicitly theological voice, but this philosopher finally looks to the church, to the saints, to clergy and to theologians to say more, to take back death and dying from medicine, and to re-imagine both our medicine and our care for the dying. That is to say, he puts the ball in our court.