The meeting in the sanctuary and the meeting in the basement
In opioid country, churches get to know their recovery communities.
When Janice Ford was called to be rector of the Church of the Reconciliation (Episcopal) in Webster, Massachusetts, she had no idea that in a few years she would be vacating her office in order to make room to house men in recovery.
Like many small cities across the country, Webster has had an opioid epidemic and few resources for responding to it. With moving boxes strewn about her office, Ford recalls how she began her ministry to addicts and those in recovery. “At the time I arrived, I wasn’t thinking that this would be our ministry. It just sort of evolved.”
Ministry in a local jail combined with an intensive educational program in addiction and recovery opened Ford’s eyes to the needs of an ignored population.
Over the past two years, Ford and the church have been creating the Reconciliation House, a house for men in recovery who are leaving the jail system and either cannot or will not return to their former living situations.
“They have no place where they can go and be confident that they can maintain their sobriety,” Ford tells me. “In some cases they are going back to the street. In some cases they are going back to a home situation that is less than optimal. Many of these young men have parents who are alcoholics and addicts. It is very hard to stay clean and sober in that environment.”
Read our latest issue or browse back issues.
In Webster, local industry dried up long ago and white-collar wealth migrated to the suburbs. The scarcity of opportunities for upward mobility is inversely matched by the easy access to drugs. Where once a drug like heroin could only be bought in Boston or Hartford, now it is found on the streets of Webster.
Last year, the leading cause of accidental death in the United States was drug overdose. In 2015, 47,055 people died of drug overdoses, and nearly 30,000 of these were caused by opioids. In Massachusetts, four and half times more people die by drug overdose than by car accident, and nearly 1,700 infants were born last year exposed to drugs. Both of these tragic phenomena can be traced to the opioid epidemic facing the state.Recently Ford received an e-mail from a local doctor informing her about the presence of bad heroin across the county. Over one weekend, the e-mail read, 12 people showed up at the hospital having overdosed on bad heroin laced with Fentanyl.
Ironically, the opioid crisis in America began with what seemed to be a solution to one of medicine’s most ancient problems: pain. Pain has always been a part of medicine, and doctors, shamans, and healers of all kinds have been tasked with alleviating it. Anyone who has stared into the eyes of a person in acute pain and seen that person willing to sacrifice any relationship, any amount of money, any extraneous body part for relief knows the power of pain. Doctors see this pain every day, and every day they encounter supplicants begging for help and a few more pills.
Since the Assyrians began extracting goo from the bulb of the poppy, the world’s most effective and widely used painkiller has been the morphine molecule. Ancient Egyptians discovered its medicinal properties, Homer and Virgil wrote about potions made from opium, Arab traders spread it across the world, and in the early 1800s Friedrich Sertürner isolated the morphine molecule from opium and named it after the god of sleep, Morpheus. Morphine’s use over the past 300 years has been spread by war, and in turn, national dependence on opium has led to armed conflicts around the world. Human history has not known a time when the morphine molecule was not valuable. The current national dependence upon opioids is just another chapter in the history of the world’s complex relationship with the drug.
In his 2015 book Dreamland: The True Tale of America’s Opiate Epidemic, Sam Quinones begins his description of opioids with the story of a medical system that saw pain prevention as a moral good. In the 1990s, the meager pain treatment practices of the previous generation were seen as inhumane. An ethical mandate to prevent pain was joined to research that suggested that patients with chronic pain have low risks of opioid addiction.
Meanwhile, pharmaceutical companies began marketing new time-released opioids as effective and nonaddictive treatments for chronic pain. The most popular of these was OxyContin. Produced by Purdue Pharma, OxyContin was marketed as a 12-hour time-released pain treatment. Posters touting OxyContin read, “Remember, effective relief just takes two.” OxyContin was ready for market in 1996. Purdue’s marketing strategy aggressively promoted OxyContin as a wonder drug, and it courted doctors with all-expenses paid trips to conferences in exotic locations.
The early research indicating nonaddictive properties turned out to be wrong. According to the National Survey on Drug Use and Health, nearly 7 million people have abused OxyContin since its inception, while Purdue Pharma has made over $31 billion of revenue from the drug. From 1999 to 2008 the prescription of opioid painkillers grew in parallel with the rise in opioid abuse and accidental opioid overdose. According to one study, 259 million prescriptions were written in 2012 for opioids, which is enough to stock every medicine cabinet in this country a few times over. By this time, a new industry had been built to meet the growing demand, “the pill mill.”
As Quinones puts it, “a pill mill was . . . staffed by a doctor with little more than a prescription pad.” Pill mills became the easiest ways for addicts to obtain prescriptions for OxyContin and other opioid painkillers like Fentanyl and Vicodin. For the aspiring entrepreneur the overhead was low: some rent, some office staff, and a doctor who was licensed to prescribe Schedule II drugs. These clinics charged a monthly fee from each patient and in turn each patient would walk out with a fresh prescription for opioids.
An investigative report by the Los Angeles Times uncovered the story of the Lake Medical pill mill. After hiring a physician, the clinic began prescribing OxyContin at an alarming rate. In a few months, the clinic had prescribed 73,000 pills, worth nearly $6 million on the street. Within a year, the clinic’s prescription rate had increased to 70,000 OxyContin pills in one month. In order to distribute more OxyContin, Lake Medical began paying homeless people to pose as patients in order to write more prescriptions. Eventually, federal, state, and local law enforcement shut down Lake Medical, and lawmakers across the country have passed legislation to curb the rise of pill mills.
Prescription monitoring programs have become popular among state legislators, and a recent study of Florida’s 2010 pill mill legislation revealed that the law saved more than a thousand lives over 34 months. New legislation is making a dent in opioid overdoses, but the lasting effect of pill mills is still felt in the increased rates of opioid addiction in the country.
As aggressive pain care and pill mills created addicts at alarming rates, a new type of drug dealer emerged to meet the growing demand for opioids. Armed with high-powered black tar heroin, a cadre of men and boys from a small town in Mexico began distributing drugs in mid-sized towns across the country. The Xalisco boys, as they came to be known, had a direct pipeline to heroin manufacturing in Nayarit, Mexico, and developed a system of drug delivery that catered to customers.
The Xalisco boys understood that convenience sells, that danger is bad for business, and that customers like a deal. So they delivered the drugs to people unwilling to come to the rougher neighborhoods where drugs are often sold on the streets; they never carried weapons or fought for turf, and they were willing to offer special deals. The dealers sold only small amounts of black tar heroin in balloons that they kept in their cheeks for easy disposal. Their story of entrepreneurial hard work sounds like most immigrant success stories, except the trade was in opioids.
The opioid epidemic touches nearly every community in the country. The faces of the epidemic include the former football player treating an old back injury, the veteran who returned wounded from Kandahar hooked on pills, and the mother suffering from chronic joint pain. The face of opioid use is also overwhelmingly white and does not easily fit into any one social class. Poor and rich alike are caught in the grip of opioid addiction. As Quinones puts it, “Children of the most privileged group in the wealthiest country in the history of the world [are] getting hooked and dying in almost epidemic numbers from substances meant to, of all things, numb pain.”
Behind the epidemic are stories, and Mike Clark, who has spent about 15 years of ministry among those in recovery, has lots of stories. Clark is a pastor at Belmont-Watertown United Methodist Church, 50 miles east of Webster. The stories he tells of addiction and recovery are full of hope and tragedy, and never saccharine or glib. “The army travels on its stomach. Addicts travel on stories,” he says.
When Clark was called to the church, it had seen better days. Previous conflicts had fractured the community, leaving behind only a faithful remnant. As Clark tells it, he would finish writing his sermon and look out his office door at all the people descending into the church basement for a recovery meeting. He would smile and wave, and people would wave back.
“There were 35 of us and a thousand of them; they were all in the basement, we were all upstairs, and if anybody was letting anybody use the building, it was the recovery community letting the church use the building.”
Clark started “loitering with intent.” He served the recovery group cider and cookies at Christmas. He met with people who needed his counsel, and he kept waving a greeting to others. He rarely if ever attended a meeting. He just spent time on the periphery. The folks in recovery started making their way to his office, and then gradually, a few to the sanctuary. In time, the congregation began looking for ways to meet the needs of the community downstairs, wondering how best to be engaged. The eventual relationship “wasn’t anybody’s idea. So, I kinda think it was God’s idea.”
Today, the church hosts nearly a thousand people in 23 recovery meetings each week. It also created the 11th step cafe, a take on John Wesley’s Class Meeting of 1745. The meeting serves as an important third space—neither church nor recovery meeting—that allows church members and those in recovery to spend time in mutual community. Recently, members of this group began telling their spiritual autobiographies to each other. After one session, a woman said to one of the addicts in the group, “You are all covered in tattoos, I have known you for four weeks, I have already told you things I haven’t told my best friends of 30 years. How’d you get us to do that?”
In many churches, avoiding honest talk is one of the fees the faithful pay for entry. Only show your best side, admit only your small sins, hide your dirty laundry, pray for the godforsaken far away, and hide the presence of the godforsaken in your own house—these are often the rules. Congregants are tempted to hide their problems like junkies hide track marks.
Both Clark and Ford say that in confronting the scourge of opioids churches need the courage to be honest. “Recovery meetings demand honesty; they don’t work otherwise,” Clark says. Honesty is integral to the salvation of the addict. The courage to meet the coming day is always accompanied by a requisite honesty to admit that the disease is never far from you.
Each week the Church of the Reconciliation prays, “God, show us the way to spread your holy word, and give us the means, courage, and stamina to follow it.”
The story of addiction in this country is a big and complex story. It is about the lies told to strengthen stigma. It is about the boasts of the arrogant that create division. It is about the craven decisions of the rich to choose profit over support. It requires us to believe that addicts are dangerous and resource-draining and should be marginalized.
Clark says that the addicts he has worked with universally love the story in John 9 of the man born blind. When the man first speaks of his healing, “he begins kind of mealy- mouthed,” Clark says, and addicts recognize him. “Oh, he is at his first meeting and he is too shy to talk. Yet, every time he talks, he talks longer, and over time, he becomes bolder. When the story starts he is lying there like a bum and everyone is talking over him. . . . Now he has a voice. And as he talks his voice gets stronger.” By the end, the man has claimed his voice and will not let the Pharisees ignore him any longer.
The ministries led by Clark and Ford are testing the hypothesis that sustained and consistent contact will lead to better understanding, deeper compassion, and less fear. Neither Ford nor Clark thinks it wise to compel people to be a part of community, and both want to preserve the boundaries between the church and the recovery meeting. Yet, by pulling the communities closer, the opportunities for relationship increase, and relationship leads to transformation both for the person in recovery and the church member. “It’s all about relationships,” Ford says with a sigh, “which take a lot of time and energy.”
This time and energy might seem wasted when the ministry flounders or the relationships can’t seem to grow. Yet ministry to those who live one day at a time requires consistency, sacrifice, and faithful commitment with a long view.
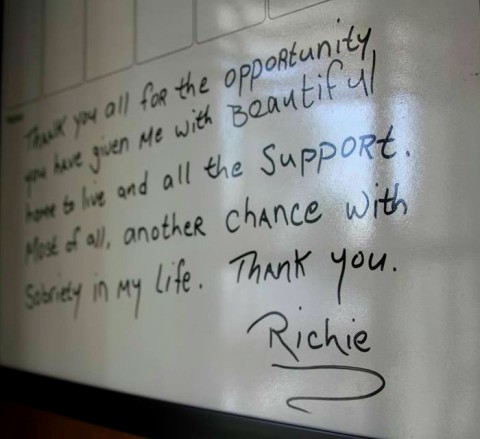
On a stewardship Sunday at Belmont-Watertown UMC, Clark says, the speaker was a person from a recovery meeting that had been meeting in the basement for years. The man told the congregation that this building had saved his life and every day saves his life again. As the man sat down to a standing ovation, he was shaken and a little embarrassed. He asked Clark, “Do they do that for all speakers?” Clark laughed and said, “They haven’t given anyone a standing ovation in 90 years.”
During the passing of the peace, a member of the church whose grandson had just died from an overdose shook the speaker’s hand and said, “If my grandson had known one person like you, maybe he’d be alive.” Clark asks, “Where does 15 years of keeping the lights on and waving lead? To these two people meeting in the passing of the peace.”
Recovery meetings have existed in church basements for decades, but the church has been happy to respect the firewall between the recovery meeting downstairs and the sanctuary upstairs. Some of this respect was born of the necessary anonymity required in the recovery meeting. Another reason for the boundary is the tacit assumption that these two communities are fundamentally different. Today, the barrier between the two communities has become more porous, and as addiction spreads, pews are filled with addicts and their families.
“People are being touched by this crisis,” said Ford. “The congregation can’t look at it as ‘those people,’ because those people are our people.”
A version of this article appears in the November 9 print edition under the title “Facing the opioid crisis.”