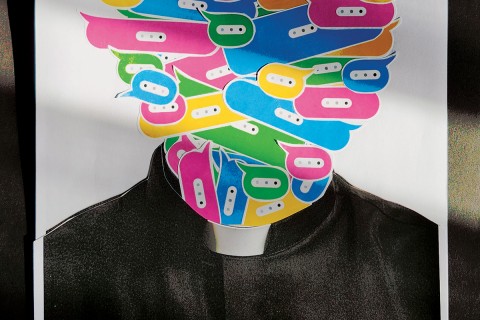
Graceful exit: My husband's choice
As a Presbyterian pastor, my husband, Bob, had always been sympathetic when a parishioner became trapped by dementia. His views on dealing with dementia had been shaped by his father, a man of deep Christian faith and an active layman. When his father began to decline mentally in his late sixties, he explained to Bob that a pattern of late-onset dementia in the family was now affecting his generation—and that his was the sixth one affected. (Only one of the six children reached 70 without mental impairment.) In his last years, Bob’s father often quoted the old axiom, “Pneumonia is an old man’s best friend.” Progressing dementia forced him to retire at 70, and he eventually had to be placed in a nursing home. Before long he began refusing food and exercise. When Bob’s mother called to report that his dad had developed pneumonia, she said she had talked to their doctor, a longtime friend, who agreed with her that there was “no point in treating the illness.” He died from pneumonia a few days later. Bob supported his mother’s decision and reassured her afterward that she’d acted in accord with his father’s wishes.
Bob’s mother enjoyed a number of active years after the death of her husband, but then she began having mental difficulties and suffered a major stroke. It was painful for all of us when she was moved to the dementia ward. When our older son visited her, he was furious. “You know Grandma didn’t want to live like this,” he protested. I did indeed know; I had even asked her if she wanted to quit taking her heart pills, but, like a good doctor’s wife, she had replied, “I think I ought to be taking them.” With no living will in place, she spent the next four years in anxious confusion until a merciful end came in her sleep. From then on my husband often said: “When I have to go to a nursing home, I will stop eating the way my father did.”
Early in his seventies, Bob realized that he, too, was falling prey to dementia. He made it clear to his doctors that he had no intention of suffering as his mother had. His physicians’ directives were in place. When he refused to take another stress test, his cardiologist agreed with him that a heart attack was an easier way to go than pneumonia. He had refused to buy nursing home insurance, telling our financial adviser that he wouldn’t be in a nursing home that long. Later, when the dementia was progressing rapidly, he balked when the dentist urged him to replace a crown.
Soon Bob could no longer read and was unable to write his name. He communicated mostly with hand gestures and at times didn’t remember who I was, but he continued to enjoy life. The love and support from our church community meant a great deal to both of us. We had joined the church after I was hired as the senior choir director, and now choir members taught me how to tie his tie. They helped him robe and brought him back if he wandered off while I was putting music away.
The day came when Bob wandered away from home and headed out on the long road through the woods to town. I found him helpless and disoriented 15 minutes later. When I told him we might have to think about nursing home care if I couldn’t keep him safe, he became tearful and pounded his knees. “I will try so hard! I will try so hard!” The immediate problem was resolved with a GPS bracelet, which Bob readily agreed to wear. I began taking him to a daycare facility for half a day each week so that I could run errands without worries. The decline continued, however, and our sons thought that I should accept a vacancy in a top-notch nursing home. (The neurologist had insisted that I put him on the waiting list at two excellent local facilities.) But when I realized how hard it would be to keep Bob involved in all the activities he still enjoyed—a monthly dinner theater group, symphony concerts, church choir, beach walks and entertaining guests at home—I turned down the opening.
At our next visits with his primary doctor and neurologist, I asked them if they thought we might be able to manage until the end with hospice help at home, and they thought it would be possible. I couldn’t bear to place Bob in a nursing home, as this might trigger his resolve to quit eating. With hospice care, I wouldn’t feel responsible for pushing Bob into fasting, and he could stay in his beloved home. When friends had asked how long we planned to live on the lakefront, his response had always been: “When I leave here, they’ll have to carry me out feet first.” I turned down three more nursing home vacancies, and then hospice announced its new palliative-care program. Now we could have hospice assistance available if we needed it, without any time frame for that care. Bob felt close to our interim pastor, and I invited him to come talk with Bob to make sure that he was indeed open to hospice care. They walked along the beach, and when they returned our pastor nodded. The next day I called hospice.
I found out about a national gene study that was recruiting volunteers from families that had two or more siblings with signs of Alzheimer’s, and Bob and his brothers, who were having similar problems, agreed to participate. All three were tested for the study by a neurologist in their area, and all three had blood drawn for a gene study. A first cousin who had no signs of Alzheimer’s agreed to be tested as the control. The brothers’ brains would be quickly harvested after death, and after autopsies, sample tissues would be sent to scientists around the world. The control blood sample might show which cells were involved in the onset of the disease. It was comforting to think that some good for others might come out of our family’s difficulties.
It hadn’t occurred to me that Bob would begin a fast right away, since he would initially be on palliative care only, so I did the weekly shopping and filled the fridge with the fresh fruits and vegetables that Bob enjoyed. When he got up the next morning, I told him I’d have his daily muesli and fruit juice ready shortly. He shook his head and waved his hand back and forth in denial. I then suggested a favorite of his, poached eggs and sausages, but he waved that offer away also. Blueberry pancakes got the same negative response. I was stunned for a moment, and then I realized that he had decided to begin his fast. I reminded him of what we had talked about months earlier. Food would always be available to him—crackers and cookies on open shelves, along with nuts, raisins, bananas, apples, etc.—but that I wouldn’t eat when he was around, thus making it easier for him to follow through once he had started. He could always change his mind, I assured him, but I would not tempt him by sitting down to eat in front of him. (I lost ten pounds that month.)
Years earlier I had fasted for ten days as a spiritual discipline, and I knew that after the first day he would probably be comfortable. This seemed to be true. We walked the beach together, swept the sand from our driveway, talked with friends and went to church that Sunday. On Monday he was switched to regular hospice care and their intake nurse visited us. Bob looked out over the lake as I told her what his plans had been and how I was proceeding. When she mentioned that a hospital bed would be provided when he needed one, I suggested that we put it in front of the picture window facing the lake. Bob visibly brightened at that, for he knew then that he would be at home until the end.
For three weeks we relaxed and enjoyed uninterrupted time together, except when I was out watering the garden. Bob could have helped himself to food, but there was never a sign that he had, or any indication of any interest in eating. I invited our retired pastor and his wife to come for a visit, and we sat out on our deck and shared memories as Bob smiled and nodded in response. Our sons and my sister visited, and I invited close friends to come for a last visit. We watched DVD movies—more than we’d seen in our 55 years of marriage. This was the house where we had spent a brief honeymoon before heading off to serve on a church camp staff, and I felt the same closeness now in these final days. How grateful I was that we could be together through the process of his departure!
When a urinary infection developed, meds seemed to keep him comfortable. We had been told that antibiotics would not be used to delay the process. The hospital bed arrived, and Bob’s devoted little cat snuggled by his feet. He gradually slipped into a coma and died after fasting from food (but not water) for 28 days.
A few days before Bob died, I found a yellowed newspaper article that he had filed with his living will ten years earlier. It described the positive experience a concerned son had when the doctor told his terminally ill mother that she didn’t need to continue eating if she was ready to go. The son described the relief and peace they both found when she was given that merciful option and could be released from her discomfort. A month later, I shared the article with a retired Christian surgeon who was giving a talk the next day on “Five Wishes,” a new booklet that helps individuals express end-of-life wishes. This document is now accepted as legal in many states. The doctor was delighted to have the article and to hear our family’s story.
He agreed that Bob had made a good choice. It was, after all, a natural death—one that would have been routine a generation or two ago. I told him that I had been uneasy about my husband’s plans earlier in the summer and had discussed my mixed feelings first with a counselor and then with our interim pastor. Now, after the special bond that Bob and I had experienced through the fast, I was grateful for his final decision. His soul was no longer trapped but was free to “graduate,” as he had so often expressed it. I had fulfilled his wishes as my final gift to him, and later I came to see his choice as his gift to me. I don’t know if he thought of it that way, but at his death I, too, was free to move on.