The coronavirus is helping us rehearse for our own deaths
“A lot of people want to talk about the big questions; they just don’t know how to get started.”

In her forthcoming book The Lost Art of Dying, primary care physician and medical ethicist Lydia Dugdale tells the story of an elderly man she calls Mr. Turner. She and her colleagues resuscitated him three times in one night, and still he died. Despite giving him the best that medicine had to offer, she felt she had contributed to his dying poorly. That led her to explore what it might mean to die well.
We might say that it is human nature to avoid conversations about death and dying, but in your book you argue that it is largely cultural.
At other times and in other places people participated much more actively than they do now in the care of a dying person. They themselves were practicing, rehearsing for their own deaths. They were reminding themselves of what they believed, so that when their time came, they were prepared.
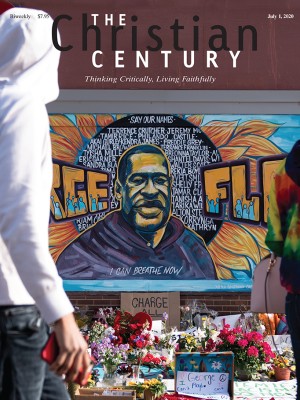
Read our latest issue or browse back issues.
That sort of community participation in the preparation for dying and death is not part of our regular activity.
Now, every day you open the newspaper and you read someone’s obituary: this person was 32 years old and healthy last week. Or this person was 72 years old and walked six miles around Manhattan just last week. Now he’s dead. Mortality is 100 percent. It always has been and always will be. But we are still surprised.
Most people conceive of a virus as something that can be taken care of medically. It’s divorced from any sense of spirituality. People ask me, “When is the vaccine coming? What are the cures? What are the treatments?” All of these solutions thwart discussions of finitude and mortality. We deceive ourselves into thinking, “What we just need is the vaccine. Then we don’t need to worry about our deaths.”
How do you see us dealing culturally with the threat that the coronavirus presents?
I’m observing that people still aren’t talking about death, they’re just getting more and more anxious. They’re hoarding supplies and stocking their shelves. There’s a certain amount of prudence in preparing for disaster; I’m not disparaging it. But fear drives us to do something rather than to sit still and reflect on what this means for life and death.
In medicine, doctors are socialized to do and not to be. That’s what we as a society expect. We want the solution, the fix, the cure. We don’t sit back and think about what we might need to do—spiritually, mentally, relationally—to prepare for death.
In your book you make the point that we look for technical solutions and assume that medicine will show us the best way to die well or live well.
Yes. In the face of this pandemic, we can see that medicine does not have all the answers. For example, many hospitals aren’t permitting visitors. Some of our very elderly patients who come in are very sick with advanced dementia. By all parameters they are unlikely to survive the disease. When they come into the hospital, they end up dying in the hospital bed with the medical team and maybe an iPad to be able to talk to their family members. That’s just heartbreaking. When you think about dying well and the coronavirus, there are many pieces to sort though. But is dying alone in the hospital bed what anybody wants for Grandma? Probably most people would say no.
There are some doctors trying to navigate these questions before their patients go into the ER, to help them know what to expect. Some older people, once they find out that their family members aren’t going to be allowed to be at their bedside if they die, are deciding against coming into the hospital. Doctors are working with visiting nurses and home hospice agencies to provide whatever medical support they need at home so they can be with their family members when they die.
That sounds tricky when we’re trying to isolate people so family members don’t also get sick.
It’s absolutely tricky.
What resources and practices can guide people of faith in this time?
There isn’t much collective ecclesial reflection on death these days. But some aspects of Christian liturgy still allow us an opportunity to reflect on our mortality. I think particularly of Ash Wednesday. The liturgy is all about dying: dying to sin, dying to self. It’s about preparing for Christ’s dying.
Churches are also getting creative in meeting the needs of people. How do we attend to the sick and the dying while also social distancing? Online resources from churches can be invaluable for those who are dying in the hospital.
We can also take a somewhat practical approach. Some people know for sure that they have had the coronavirus. If that’s the case, those people may be more equipped to serve. Then there are young people without any medical problems, who are likely to emerge from this fairly unscathed. As has always been the case, the healthier and more robust have been able to serve those who are sick and infirm.
A number of my medical students, for example, have organized within their buildings in New York City to purchase food and pharmacy items on behalf of the elderly and sick. Why not pick up groceries for an elderly neighbor? You still wash your hands when you come home.
In a recent op-ed in the New York Times, a doctor said that even hospital staff try to spend as little time as possible with coronavirus patients, not wanting to “share the same air” with sick patients. How have you managed these fears in your own work?
There is a conversation right now in medicine about whether doctors and other first responders like nurses should be expected to be willing to give up their lives. Does society owe them anything in return? For example, we don’t send folks into military service without equipping them. Is it fair to expect doctors and nurses to work the front lines without protective equipment?
I’ve held the view that I’m willing to serve even if it means my life. My calling into medicine was so strong it was inescapable. Having said that, I’m a healthy person. The odds are I’ll be just fine. It’s a lot more to ask someone who suffers from chronic illness to have that same equanimity. I don’t begrudge those individuals who have chosen not to come to work. I can only know what the call is on my own life.
Death has always been part of our family conversation, including with my children. I’ve been very honest with them that there’s no guarantee that any of us will get to the other side of this pandemic and still be alive. We talk very openly about how that will be difficult, but we’re not without resources for handling that, spiritual and relational. One of our constant refrains as a family has been, “We need to treasure this time. We need to treasure our relationships. We don’t know how many days we have together. We need to be grateful and care well for one another.”
What is important for us to be doing now to prepare for our own deaths or the deaths of people we know? What conversations should we be having, especially with older people in our lives?
It starts very simply. Ask, “Who should make medical decisions for you if you become too sick to decide for yourself?” Choose someone and put it in writing. From that conversation, then, flows, “Have you thought about what you would want the end to look like?” It’s possible to die in a hospital, possible to die at home. Possible to die on life support. Start to have those conversations.
A lot of patients, even without much knowledge of how health care works, still have a sense of these big picture questions. Hospital or home. Life support or not. Tube in my throat, where I can’t talk but it’s supporting my breathing, or not. Somebody checking my blood work and vital signs every two to four hours or not. Some people who have spent any amount of time in a hospital get to the point where they just don’t want that anymore.
These practical questions can start to push conversations gently toward the so-called big questions. How do we want to think about a funeral? What songs would be sung? What texts would be read? Who would speak? If you start to think through this, it puts a lot of things very quickly into focus. You start to identify what your values are, what you believe, what you profess. There are a lot of people who want to talk about this, they just don’t know how to get started.
What are you praying these days?
French theologian Jean-Claude Larchet said that in times of suffering we should not pray, “make this go away,” but, “may that which is most spiritually useful transpire.” That’s what I pray: health, safety, and courage, and where those are not possible, may the most spiritually useful thing be done.
What are the spiritually beneficial outcomes you would hope to see from this crisis?
That people face their finitude more squarely. If dying well requires living well, there should be a fundamental recalibration of how we live. We need to give our full attention to what ultimately matters.
A version of this article appears in the print edition under the title “Rehearsing for our death.”