Healing hands
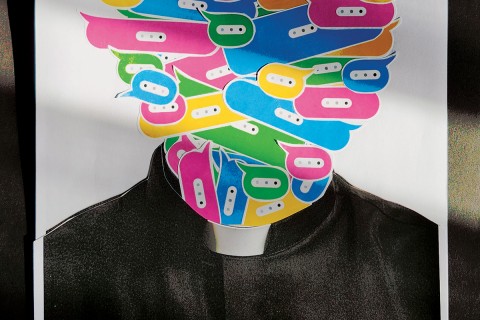
When my 90-year-old father fell at home a few months ago, a trip to the emergency room revealed that he was shaken and dazed by the experience but not seriously injured. A follow-up visit to his clinic, however, turned into an unexpected piece of medical theater. The doctor entered the examining room with two lab-coated medical students in tow. From the threshold, he greeted my father, who was perched anxiously on the examining table, and then immediately turned to a computer in the corner of the room. After conferring with the students for a moment about the data on the screen, the physician looked toward my father. “Labs look OK. If you have any complications, give me a call.” Then, like white-winged waterfowl flapping away from a pond, the medicos were gone.
A rushed and harried teaching day for the physician? Probably. But even so, this reflects a troubling trend in contemporary medicine. In one corner of the room were the facts of the case, the data flashing on a computer screen. In the other corner of the room was the patient, the human being, shivering, perplexed and untouched.
Read our latest issue or browse back issues.
Lewis Thomas, the late dean of Yale Medical School, once observed that although younger physicians today are superbly trained, they often lack two essentials. First, as children of the antibiotic era, most have never been sick and thus cannot truly empathize with their gravely ill patients. Second, in focusing on the tools and techniques of scientific medicine, they have forgotten that all healing derives from human touch. “The doctor’s oldest skill in trade was to place his hands on the patient,” Thomas said. People who are sick long to be touched, which ironically is the very thing that even close friends and family often avoid. In today’s mechanized medicine, doctors, too, are prone to keep their distance. “Medicine,” said Thomas, “is no longer the laying on of hands, it is more like the reading of signals from machines.”
A refreshing counter to this trend has now appeared in Victoria Sweet’s memoir, God’s Hotel: A Doctor, a Hospital, and a Pilgrimage to the Heart of Medicine. In her early career, Sweet was solidly convinced of the power of scientific medicine but also increasingly aware of its limitations. She sensed deep levels of communication with her patients that transcended the usual data and diagnoses. In moments of birth and death, in key turning points in an illness, there was, she noticed, “evidence of some subtle but shared world . . . invisible connections with visible effects.” A search of the medical literature for explanations was disappointing. Such phenomena had not only been given boring labels—the “doctor-patient relationship,” the “placebo effect”—but they had also been psychologized, separated from the body where Sweet had seen and felt them.
Sweet turned for deeper understanding to a source from her own faith tradition, Hildegard of Bingen, the 12th-century mystic. Hildegard not only experienced visions and composed ethereal music, she also served in her convent infirmary as a caretaker of the sick. She touched fevered foreheads, took urine samples, measured pulse rates and wrote about it all in a medical manual. Through medicine, Hildegard’s reveries found a place of embodiment. She was not only “stunned into silence by a vision of the universe,” writes Sweet, but also “knew how to prepare a potion and touch a patient.”
Sweet joined the staff of Laguna Honda, a San Francisco almshouse hospital for indigent and homeless patients—what the French call a “hotel of God.” Here Sweet was free to augment scientific medicine with what she learned from Hildegard. She began paying attention to patients’ anima—not the abstract, disembodied soul but “the invisible force that animates the body, that moves it.” Patients who had been viewed as hopeless responded with surprising vitality when Sweet began seeing their bodies as an oikos—an ecology of spirit and biological process. Touching the sick became not merely a means to probe for a diagnosis but a way to impart a blessing.
In a time of understandable anxiety about “safe touch” and “proper touch,” I want to remember Hildegard’s lessons and not lose sight of the deep power of healing touch. The health-giving gesture of the physician’s hand derives, after all, from the more ancient ritual of the priestly blessing. Psychologist Paul Pruyser once said that at the close of a therapy session there is often an awkward moment. Both the patient and the therapist yearn for the very thing secular therapy prohibits—a placing of the hand of blessing on the head and the pronouncing of a benediction.
Lewis Thomas remembers as a boy going on house calls with his physician father. Whenever his father visited one particular patient, he would always park his car a block away and around the corner. This patient, his father explained, was a Christian Scientist, a pillar of his church, and could not afford to be seen consulting a doctor. But, Thomas says, if people had known the kind of attentive, touch-centered medicine my father practiced, he could have parked his car right out front, because “it was, in its way, faith healing.”